Most communities approach options for adopting major upgrades in local medical care with an eye aimed towards critical systemic dynamics and engagement with key members of their local medical community. For example, consider the process McKenzie-Willamette Medical Center undertook roughly three years ago when they first started exploring serious interest in implementing an approach to orthopedic surgery that embraced modern robotics as the centerpiece of surgical knee and hip repair.
The catalog of questions needing answers was long and demanding. And the stakes weren’t low. Knee and hip replacements top the list of most frequent surgeries in the Eugene-Springfield area, as in many communities across the U.S. And all surgeries, whether common or relatively rare, come with their own special considerations.

“Everything is moving toward minimally invasive service,” says Jana Waterman, McKenzie-Willamette’s vice president of business development. Waterman was intimately involved in McKenzie-Willamette’s decision to adopt robotic orthopedic surgery as a standard option for patients. Her priorities included positive patient outcomes. Pain management. Post-surgery medication needs. Patient satisfaction. “Surgery is no longer about opening up the patient,” she explains. “How can we do surgery with the least amount of intrusion into the body? That’s where medicine is heading.”
According to Waterman, people often hear about the newest medical approaches, then take their interests to their personal physicians and local hospital administrators. McKenzie-Willamette considered patient interest in their decision-making about orthopedic robotic surgery. They also mined the experience and research of leading-edge medical institutions like Stanford and the Mayo Clinic, and contacted surgeons at Eugene’s respected Slocum Center for Orthopedics & Sports Medicine. Also in the mix was an interest in recruiting younger, recently graduated orthopedic surgeons trained in the most modern robotic techniques.
Three years ago, McKenzie-Willamette had no direct experience with robotic orthopedic surgery. They did however have experience in using the da Vinci Surgical System, which provides robotic assistance for general, colorectal, cardio, gynecologic, and urologic surgery (not orthopedic surgeries).
McKenzie-Willamette ultimately decided to adopt the much-respected orthopedic surgery system fronted by Mako robots, made by a company called Stryker. In this case, actually, two Mako robots. At the relatively young age of 7, Mako is the oldest, best-established orthopedic robot with combined capabilities for performing both hip and knee replacement surgeries. It is a standard-setter for effectiveness and quality.
The decision to go with Mako was driven to a notable degree by Mark Mildren and Lucas Korcek, a pair of young orthopedic surgeons on Slocum’s staff. The two surgeons were ultimately recruited and contracted by McKenzie-Willamette for their knowledge and skill at using the Mako robot. Today they are the only surgeons doing joint replacements using Mako in the Eugene-Springfield area.

Da Vinci and Mako have some similarities but also key differences.
“Think of da Vinci more like a video game,” says Mildren. “You’ve got the game that’s actually taking place in one location over here, but you’re controlling procedures in a different location back here. You’re still controlling everything with your video game controllers and pinchers, but the real action is what’s taking place at the surgical site over there.”
Da Vinci is different from Mako because the da Vinci allows the robotic arms to get into places that normal arms usually cannot. Robotic orthopedic surgery, on the other hand, is more about using the robot to make precise cuts in the bones, Mildren says. “I’m in there doing the cuts with the saw,” he explains. “It’s just that the robot is controlling where the saw goes. That’s the difference between da Vinci – which allows for minimally invasive stuff – and Mako, which allows for better precision where your cuts go.”
McKenzie-Willamette’s Mako system is programmed to function collaboratively. The surgeon maintains control of the robotic saw at all times. The Mako provides guidance by indicating the precise plane on which to position the saw. It also sets virtual boundaries that prevent the saw from moving outside of safe parameters. This interactive approach ensures surgical accuracy while allowing the surgeon to leverage the benefits of robotic assistance. With the Mako, the surgeon can make meticulously precise cuts that would be impossible through manual methods alone.

“I hold the robotic saw and guide it where I want it to go, with the Mako advising me on the optimal angle and depth,” says Mildren. “By working together with the technology, I have the precision of robotics with the oversight and expertise of an experienced surgeon.”
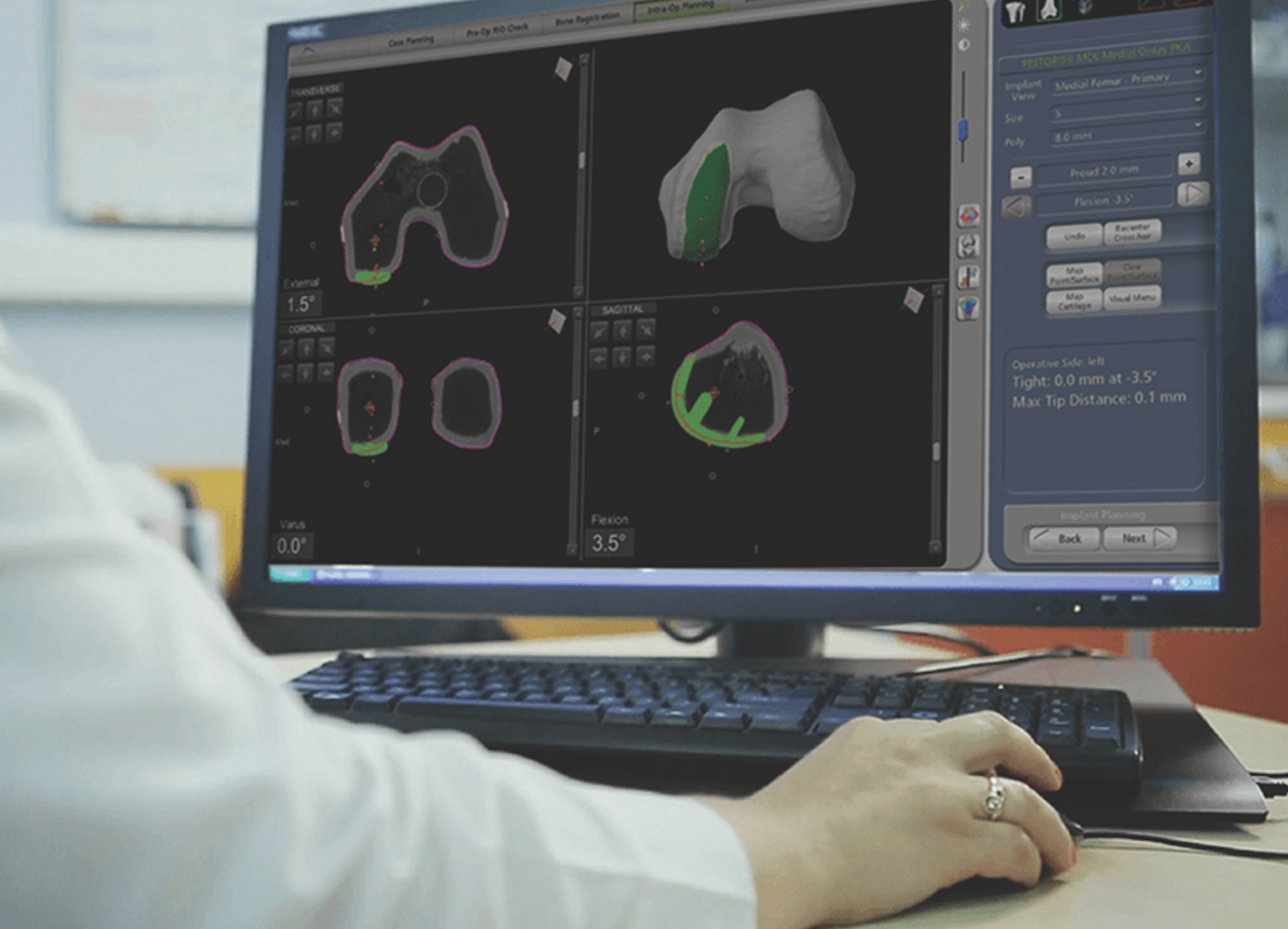
One unique feature of Mako surgery is the use of a pre-op CT scan to compose a scalable 3D image of the surgery site. The image plus computerized operational data are used by the robot to construct a surgical plan that includes procedural steps, maps depicting incision points, and highly specific measurements that steer the surgeon through the full surgical process. Mako plans even allow for mid-process adjustments and image modifications reflective of real-time changes in surgery conditions.
There are many important points of comparison when reviewing the advantages and disadvantages of performing Mako-assisted surgery versus what is generally referred to as traditional hand’s-on joint replacement surgery. Put another way, what might you likely hear from a patient who has undergone a Mako surgical experience? Does their view reflect the most commonly promoted post-op perspectives available to patients seeking knee or hip replacements?
“I’m no spring chicken,” confesses Holly Frei, a sharp-witted 81. About a year and a half ago she started experiencing unbearable pain in both her hips. “I was in so much pain I wasn’t sure if life was still worth living much longer if I couldn’t get help.”
She found help after spending several months researching, then getting an appointment with Dr. Mildren. He scheduled her for replacement surgery on her right hip in the summer of 2023.
“I didn’t feel there was really a choice as to robotic or traditional surgery,” Frei recalls. “That’s what Dr. Mildren does — the robotic method — and I wanted to go with Mark.” She “did a lot of personal research,” and “everything that I found out about robotics I saw as working to my advantage,” Frei says, nodding. “One of the big things was that it offered a shorter recovery time. And the procedure was more precise.”
Frei recently set a date for a second Mako hip replacement — her left hip this time. She says her Mako post-op recovery was quick and easy, with pain from the surgery barely a concern after only four days. As a veteran patient of Mako surgery, Frei happily offers up firm opinions for others who might be considering similar undertakings.
“Do your research and then go for it,” she urges. “It’s the best thing out there!”